PSYCH Symposium is returning at the British Museum on 6 July, when a panel of experts will discuss how psychedelics could innovate eating disorder care.
With the prevalence of eating disorders increasing by 140% in the last 10 years, there is a desperate need for innovative approaches to eating disorder care.
PSYCH Symposium’s panel, ‘Treating Eating Disorders: Building Patterns & Reducing Prevalence’ will explore how psychedelics can create potential mechanisms for the brain to cope with the key triggers of such conditions.
We spoke to panel members, Professor Rebecca Park, Associate Professor & Honorary, Consultant Psychiatrist at Oxford University and Yoel Golbert, Co-Investigator at Sheba Medical Center Department For Eating Disorders, ahead of the event to find out more.
What does the current landscape look like for eating disorder treatment and what does current research show about the potential of psychedelics as a supportive treatment for such conditions?
R & Y: Anorexia Nervosa (AN) has the highest morbidity and mortality of any psychiatric disorder and is arguably the most challenging psychiatric disorder to treat, with no proven drug treatment of benefit.
There is evidence for specific forms of psychological treatment (in particular a specific Family-based treatment in adolescents with a short duration of illness, and CBT-E/MANTRA in adults ill less than 3 years and not severely underweight ). However sadly around a third of adults do not recover fully and a further third remain stuck in their illness at huge cost to lives, families, and healthcare systems.
AN also has high levels of Comorbidity, especially with OCD, Depression and Anxiety disorders, which need treatment in their own right. Thus, innovation to develop novel evidence-based treatment is urgently needed.
Current research into psychedelic therapy for ED is novel, with a cautiously emergent evidence base.
In particular, preliminary results from open trials suggest that psilocybin-assisted psychotherapy can help alleviate ED pathology in those with AN. While this is encouraging, it needs to be proven in controlled trials.
Further research into mechanisms of effect, patient selection, and the role and format of therapeutic support is also urgently needed. Clinical trials need to balance the delicate risks of benefits vs harms, especially of short-term interventions, as the road to recovery from AN is long and hard, commonly taking several years.
What are the potential risks, challenges and benefits of using psychedelics as a therapeutic tool for individuals with eating disorders? What are your thoughts on how any challenges or risks can be tackled?
R & Y: The risks, challenges and benefits stakes are highest for individuals with AN. Risks are especially high for those severely underweight and/ or binge purging, who are often physically and emotionally fragile and have medical complications which need to be taken into account.
These patients need particularly high levels of monitoring, support, and containment in the journey through a psychedelic experience. Many will have been relatively cut off from intense emotion and their appetites, due to deficits in interception and body awareness for years or even decades.
Difficulties in emotional regulation are common in those with eating disorders, whose eating disorders behaviours such as extreme dietary restriction paradoxically can serve as a protective mechanism, a means to disconnect from overwhelming core emotions.
Experiencing intense emotions and appetites as part of a psychedelic experience may thus be frightening or overwhelming to them if not expertly contained and supported. Patients need ongoing trusted support through their journeys and it is essential practitioners and researchers are mindful of these risks.
If not supported through this, patients may experience the start of the process of recovery as getting worse, rather than part of a process of getting better- and will be at risk of retreating back into ED behaviours as a way of coping.
How do psychedelics impact body image perception and self-esteem, which are often distorted in individuals with eating disorders?
R & Y: Psychedelics alter the perceptual experience and is hypothesised that MDMA and psilocybin may serve as an empathogen, reducing self-criticism whilst inducing a sense of compassion and connection to the self and others. This in turn might harness a self-perspective that is later worked on in integration and therapy. Widening the “window of tolerance“ of complex and overwhelming emotions may also foster a better foundation for therapy and nutritional support. This is crucial in a patient population that is notoriously ambivalent to treatment.
In Anorexia especially, body image is very strongly related to self-evaluation, self-image and self-esteem. Therefore, the hope would be that a more compassionate perspective of the self and of the body can in turn promote motivation and support recovery. Psilocybin can induce new insights, and enhance a sense of embodiment and personal meaning.
These effects might potentially help improve insight and body image in those with AN, who often have deficits in interoception and lack a sense of embodiment.
Are there any specific psychedelics that have shown promise in addressing the underlying psychological factors contributing to eating disorders?
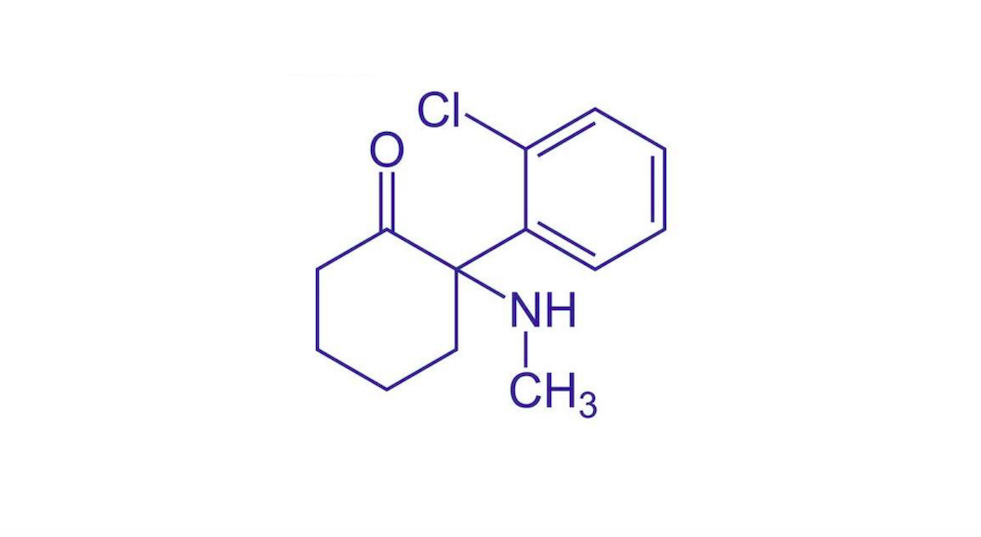
R & Y: Regarding peer-reviewed research, data is still emergent, with several studies in progress. Psilocybin has shown some benefit from preliminary findings of open studies and has a good safety profile, which is important, especially in AN.
Controlled trials are now underway in AN. Evidence from studies such as depression suggest psilocybin can enhance flexibility, openness for change, reduce rumination and improve cognitive flexibility and sociability.
These effects could provide a strong foundation for additional therapeutic strategies in AN. Studies of MDMA in eating disorders are now underway, given it was found to reduce self-reported ED symptoms in an open study of PTSD .
Its anxiolytic-pro-social effects could also potentially provide a strong bedrock for adjunctive psychotherapies.
PSYCH Symposium’s panel ‘Treating Eating Disorders: Building Patterns & Reducing Prevalence’ will also include panel member Rivki Stern, CEO at Short Wave Pharma – a sponsor PSYCH Symposium sponsor – and moderator Claudia Canavan, Health Editor at Women’s Health.
To book your tickets, visit https://www.psychsymposium.com/tickets.