While a number of states have begun to legalise the medical use of certain psychedelics, widespread legalisation is set to start taking place from 2021 onwards. The new global psychedelics industry will be poised to result in cost savings of hundreds of billions annually on medication, counselling and lost productivity – entirely disrupting the way the world approaches mental healthcare.
For millennia, psychedelics have been used as both a spiritual and mental health therapy across the world indigenous communities. Between the 1940s and the 1960s, many of these drugs entered the Western academic and scientific mainstream demonstrating exceptional potential in treating mental health illnesses such as treatment-resistant depression and anxiety. However, even after thousands of patients were treated in pilot programmes and hundreds of scientific papers were published, the US government, followed by the rest of the world, criminalised psychedelic drugs and outlawed many of the research programmes examining its effects. Now, decades later, as we witness an international renaissance in clinical trials, scientific research and commercial investment, we examine the potential cost savings of legal psychedelic-assisted therapies.
The psychedelics renaissance
Restrictions brought about by COVID-19 have caused the world to renew its focus on mental health. Already a major concern for charities and health organisations, COVID-19 has further increased the call to acknowledge and treat sufferers. In addition, many of the frontline staff working in healthcare are likely to experience PTSD as a result of their dealing with the virus and will need psychological support to address this.
However, in a world facing certain recession and a possible increase in depression cases, there is a very real risk that mental health welfare will fall by the wayside as a prohibitive cost placed on an already over-stretched society. Here is where the use of psychedelics for the treatment of mental health is likely to form a very significant element of the next step forward.
A mental health pandemic
Beyond the current crises, it’s estimated there are upwards of 300 million people worldwide with depression at any one time. In addition, it’s estimated that one-third of those patients are ‘treatment-resistant’ which means current medication does little or nothing to help. Treatment-resistant depression is one of the most common mental health conditions in the world.
Thanks to a wave of new studies, scientists are ever more interested in how psychedelic drugs can be used to treat mental health conditions. These include both naturally derived plant-based varieties (entheogens) such as psilocybin, ibogaine, ayahuasca and mescaline, along with those synthetically manufactured, such as LSD, ketamine and MDMA.
Societal costs of psychedelic-treatable diseases
The potential of these psychedelic drugs to transform mental health treatments is vast. However, due to a lag in research of over 30 years, data on the use of these drugs is still preliminary. To get an idea of how valuable these drugs could be to our societies, we have calculated the potential of these drugs to relieve some of the economic burden of mental health issues. When assessing the value of new treatments to society, it is necessary first to work out how much an illness costs a society. This is done by health economists who take into account factors including:
- Direct medical costs such as the services and goods that are used or lost in managing diseases, from prevention to healthcare expenditures
- Direct non-medical expenses such as informal care and social services
- Indirect costs such as loss in days of work or loss of productivity for other reasons.
Our calculations take into account the preliminary success rates of psychedelic medicines in randomized controlled trials for mental health conditions and open-label studies for substance abuse, the direct and indirect costs to society of those conditions in given regions as assessed by medical economists, and the willingness of the public to take psychedelic medicines according to YouGov.
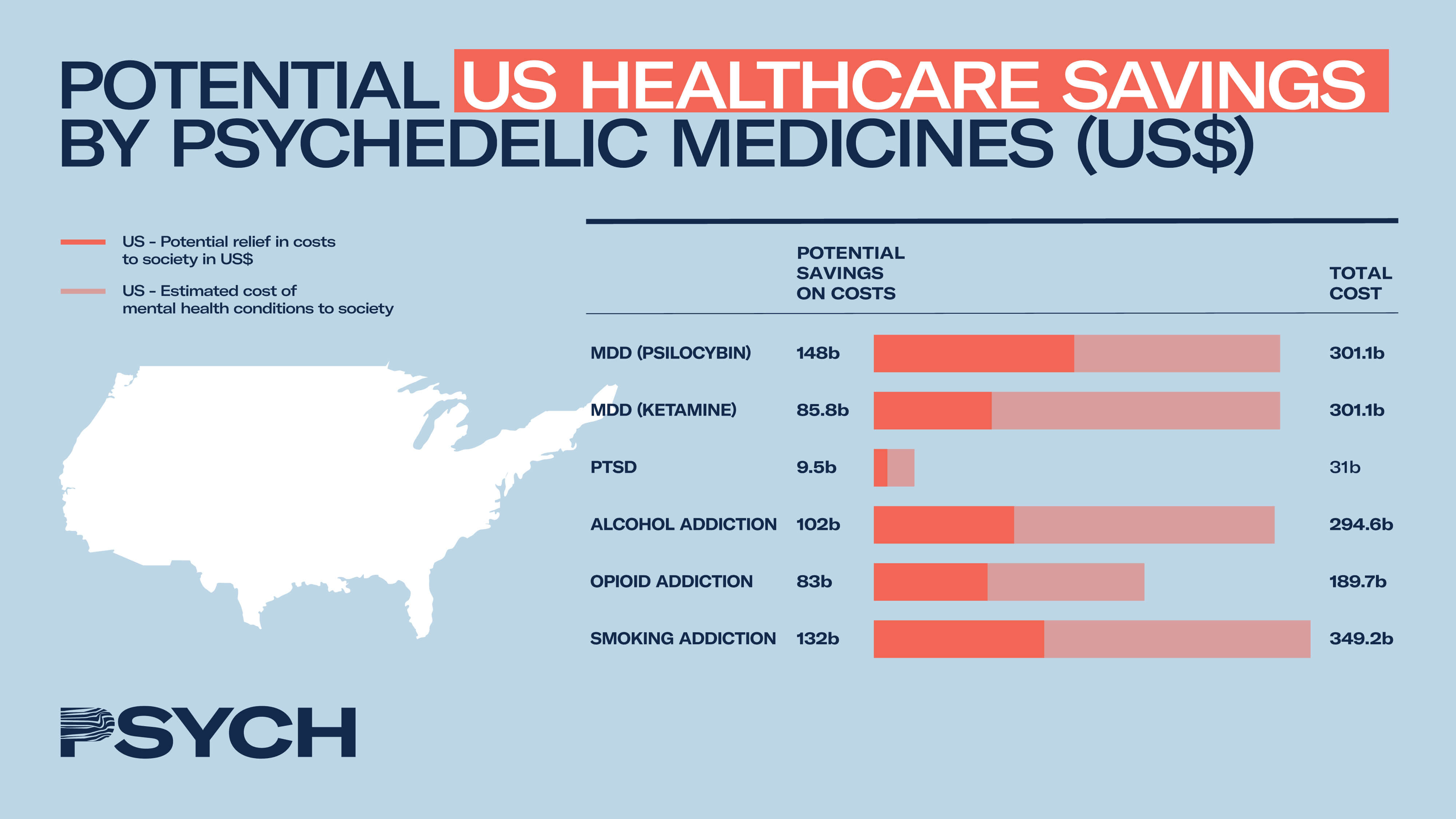
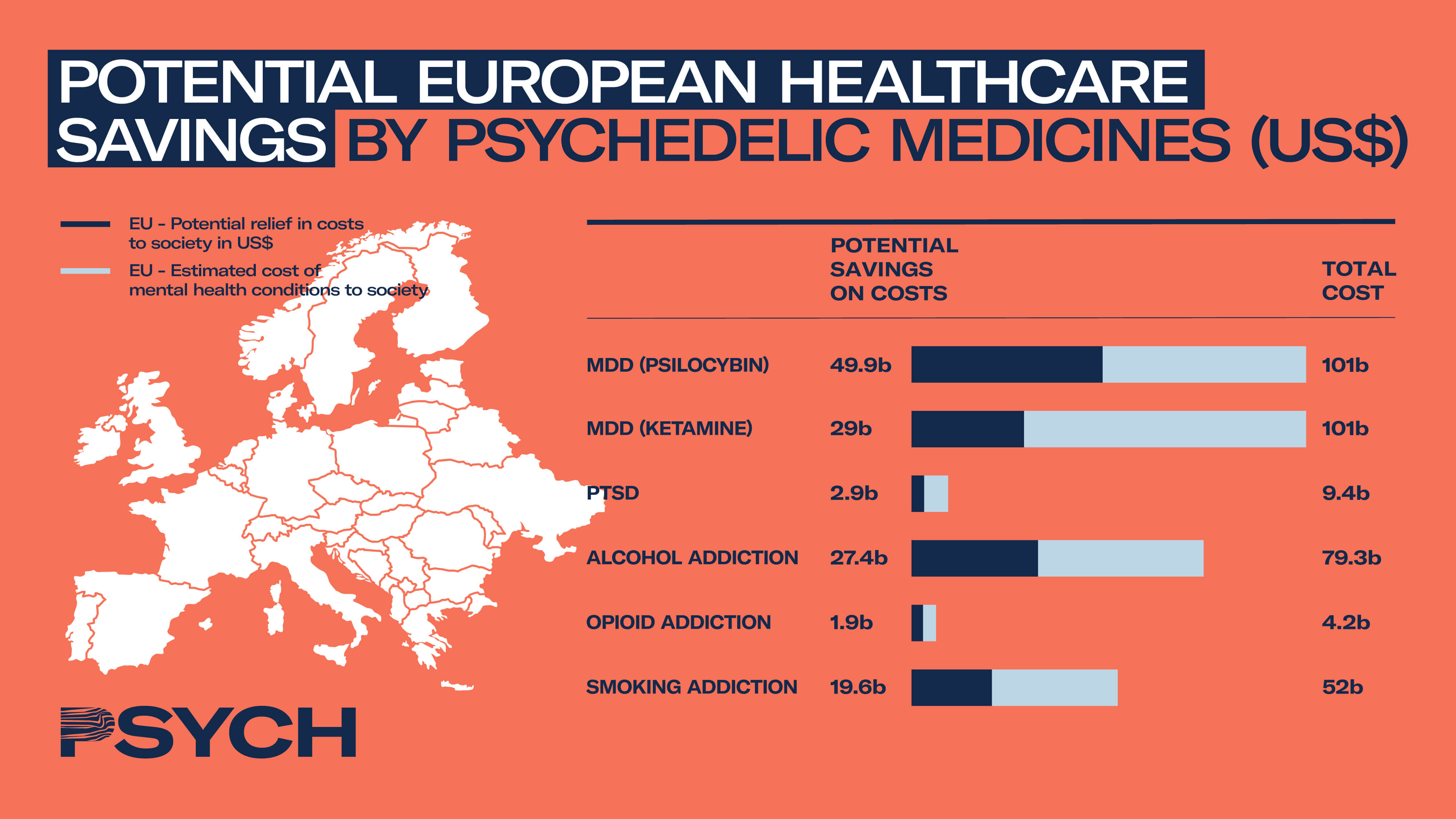
The precision of these calculations is limited primarily by the preliminary nature of the clinical data but also by the variability with which researchers assess clinical conditions such as depression and substance abuse. There also exists variability in how medical economists calculate the economic burden of diseases to society. Data for Europe relate to the EU27 as well as Iceland, Norway and Switzerland. Assumptions have been minimised but are still present in the model, for example assuming the same proportions of EU inhabitants are willing to try psychedelic medications as those in the US.
The figures are an attempt to display the economic benefits that could be wrought from psychedelic drugs if the success seen in preliminary clinical studies carries through to the medicinal market once legalised. The calculations do not include any new costs introduced by psychedelic medicines, as these are yet largely unknown but are predicted to be orders of magnitude lower than the current economic burden of these diseases.
While further clinical data and regulatory clarity will help to provide a clearer picture of the future savings of legal psychedelic medicines, initial modelling has shown enormous potential to relieve the economic burden of mental health illnesses across treatment, addiction and lost productivity. Psychedelic medicines are almost certainly set to disrupt the way we tackle current and future mental health pandemics, which are set to worsen before they get better, but as states and countries begin to roll out new pilot programmes, clinical trials, patient data and the voices of industry experts will be critical in driving forward change and normalising psychedelic treatments.
For more information on the global psychedelic medicine market or support growing your business in the emerging psychedelics industry, please contact info@psych.global


